Continuous Glucose Monitors (CGMs) have revolutionized diabetes management, providing real-time insights and improving glycemic control. At GNS Medical, we’re dedicated to helping patients access these life-changing tools while ensuring they meet the necessary coverage criteria.
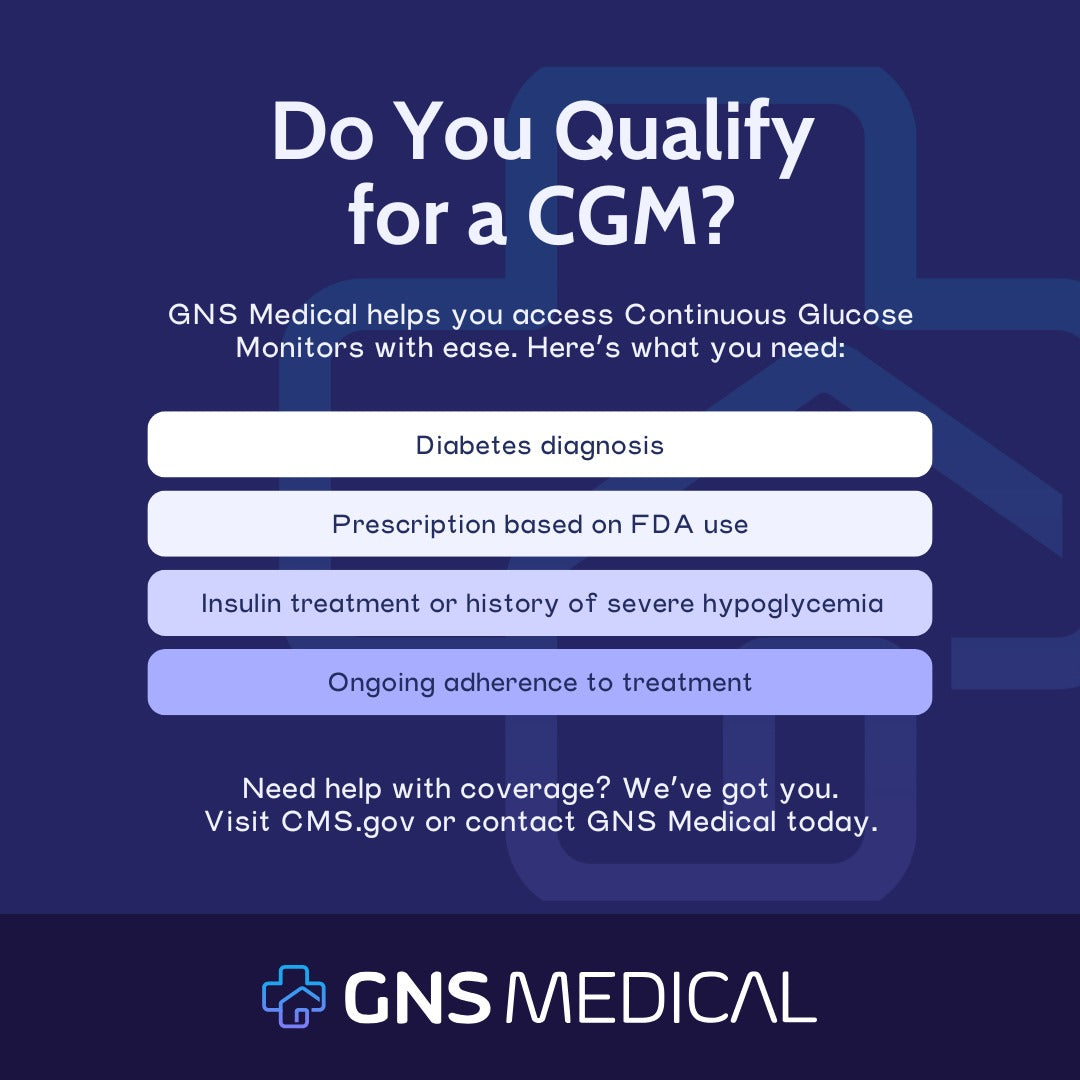
So, what qualifies for CGM coverage? Here’s an overview based on CMS.gov guidelines:
Initial Provision Requirements
To qualify for a CGM, patients must meet the following criteria:
· Diabetes Diagnosis: The patient must have a confirmed diagnosis of diabetes mellitus.
· Training in CGM Use: Evidence of appropriate training for CGM use is required, typically shown through a prescription.
· FDA-Indicated Use: The CGM must be prescribed in line with its FDA-approved indications for use.
· Glycemic Control: The device should be prescribed to improve glycemic control for insulin-treated patients or those with a history of problematic hypoglycemia.
· History of Problematic Hypoglycemia
For patients with non-insulin-treated diabetes, a documented history of problematic hypoglycemia may qualify them for CGM coverage:
Recurrent Level 2 Hypoglycemia: Glucose levels below 54 mg/dL, supported by:
· Specific glucose readings from testing events,
· A BGM testing log indicating qualifying events, or
· A documented history of medication adjustments leading up to the most recent event.
At Least One Level 3 Hypoglycemia Event: Documentation must include:
· The glucose value during the event,
· Classification of the episode as Level 3, or
· Evidence of third-party assistance required for treatment.
Ongoing Provision Requirements
Once a CGM is provided, continued coverage requires:
· Adherence to Treatment: Proof that the patient remains committed to their diabetes treatment plan.
· Regular CGM Use: Evidence of consistent device usage to monitor and manage glucose levels.
Learn More
For additional details, consult the CMS Local Coverage Determination (LCD) and related documentation guidelines (A55426) on CMS.gov.
We’re Here to Help
Navigating CGM qualifications can be complex, but you’re not alone. GNS Medical is here to guide you through the process and support your patients every step of the way.
Contact us today to learn more about CGM qualifications and how we can help!